

Neurofeedback therapy targets the symptoms of Parkinson's disease by focusing on enhancing brainwave patterns associated with motor control and cognitive function. Neurofeedback Specifically, neurofeedback aims to address the abnormal brainwave patterns commonly observed in Parkinson's patients, such as excessive beta wave activity and reduced alpha wave activity in the motor cortex. By training individuals to modulate these brainwave patterns, neurofeedback therapy seeks to improve motor function, reduce tremors, and alleviate cognitive symptoms associated with Parkinson's disease.
In Parkinson's patients, neurofeedback therapy aims to address specific brainwave patterns, such as excessive beta wave activity in the motor cortex and reduced alpha wave activity. By targeting these aberrant brainwave patterns, neurofeedback seeks to modulate neural activity and restore more balanced and optimal brain functioning. Neurofeedback Training This may help improve motor function, reduce tremors, and alleviate cognitive symptoms in individuals with Parkinson's disease, ultimately enhancing their overall quality of life.
Neurofeedback therapy has shown promise in improving motor function and reducing tremors in individuals with Parkinson's disease. By training patients to modulate their brainwave patterns, particularly beta and alpha waves, neurofeedback may help enhance neural regulation and improve motor control. This can lead to reduced tremors and better overall motor function, contributing to improved daily functioning and mobility for Parkinson's patients.
Skin Temperature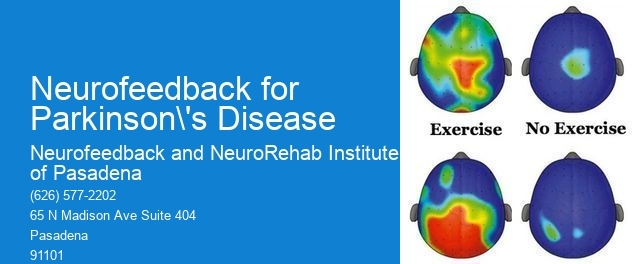
Specific neurofeedback protocols and techniques have demonstrated particular promise for Parkinson's patients, such as sensorimotor rhythm (SMR) training and alpha-theta training. SMR training aims to enhance sensorimotor rhythm activity, which is associated with motor control, while alpha-theta training focuses on promoting relaxation and cognitive function. Mindfulness These targeted protocols have shown potential in addressing the specific symptoms and neural dysregulation associated with Parkinson's disease.
Neurofeedback therapy can integrate with other treatments for Parkinson's disease, such as medication and physical therapy, to provide a comprehensive approach to symptom management. When combined with conventional treatments, neurofeedback can complement the effects of medication by targeting neural dysregulation and enhancing motor control. Additionally, integrating neurofeedback with physical therapy can offer a holistic approach to improving motor function and mobility in individuals with Parkinson's disease.

Incorporating neurofeedback into a comprehensive treatment plan for Parkinson's disease may yield potential long-term benefits, including sustained improvements in motor function, reduced tremors, and enhanced cognitive function. By addressing neural dysregulation through neurofeedback therapy, individuals with Parkinson's disease may experience lasting improvements in their overall quality of life, contributing to greater independence and well-being over time.
Heart Rate CoherenceWhen considering the use of neurofeedback in individuals with Parkinson's disease, specific considerations and contraindications should be taken into account, such as disease stage and medication interactions. It is essential to assess the individual's disease progression and consult with healthcare professionals to determine the suitability of neurofeedback therapy. Additionally, potential interactions between neurofeedback and medication regimens should be carefully evaluated to ensure the safety and efficacy of incorporating neurofeedback into the treatment plan for Parkinson's disease.
Neurofeedback therapy has been shown to have a positive impact on depressive symptoms in individuals by targeting specific brainwave patterns associated with mood regulation and emotional processing. By utilizing real-time monitoring of brain activity and providing feedback to the individual, neurofeedback therapy aims to train the brain to self-regulate and optimize its functioning. This process can lead to improvements in mood, emotional stability, and overall well-being. Research has indicated that neurofeedback can modulate neural networks related to depression, such as the prefrontal cortex and limbic system, promoting more adaptive patterns of brain activity. Additionally, by addressing underlying neurological dysregulation, neurofeedback therapy may offer a promising approach for individuals with treatment-resistant depression or those seeking non-pharmacological interventions. Overall, the targeted and personalized nature of neurofeedback therapy holds potential for alleviating depressive symptoms and enhancing mental health outcomes.
Neurofeedback has shown promise in addressing specific phobias such as agoraphobia by targeting the underlying neural mechanisms associated with fear and anxiety. By utilizing real-time monitoring of brain activity and providing feedback to the individual, neurofeedback can help regulate and retrain the brain's response to fear-inducing stimuli. This process involves enhancing self-regulation of neural networks, promoting relaxation, and reducing hyperarousal, which are all crucial in managing agoraphobia symptoms. Through repeated sessions, neurofeedback aims to modify maladaptive neural patterns, leading to improved emotional regulation and reduced phobic responses. Additionally, neurofeedback may also enhance cognitive flexibility and resilience, contributing to a more comprehensive approach in addressing agoraphobia.
Neurofeedback therapy has shown promise in addressing the specific needs of individuals with complex trauma histories by targeting the dysregulated neural networks associated with trauma-related symptoms. By utilizing real-time monitoring of brain activity and providing feedback to the individual, neurofeedback therapy aims to modulate neural oscillations, enhance connectivity within the brain's networks, and promote self-regulation. This approach can potentially help individuals with complex trauma histories in managing symptoms such as hypervigilance, emotional dysregulation, and intrusive memories. Additionally, neurofeedback therapy may contribute to improving cognitive functioning, emotional resilience, and overall well-being in this population. The personalized nature of neurofeedback training allows for tailoring the intervention to the unique needs and experiences of individuals with complex trauma histories, offering a potentially valuable adjunct to traditional trauma-focused therapies.
Neurofeedback, also known as EEG biofeedback, has shown promise in alleviating symptoms of generalized anxiety in teenagers. By providing real-time feedback on brainwave activity, neurofeedback aims to train the brain to regulate its own functioning, potentially reducing anxiety symptoms. Studies have indicated that neurofeedback may help improve emotional regulation, attention, and cognitive flexibility, all of which are relevant to managing anxiety. Additionally, neurofeedback sessions often involve relaxation techniques and mindfulness practices, which can further contribute to reducing anxiety symptoms. While individual responses to neurofeedback may vary, it is worth considering as a non-invasive and drug-free option for addressing generalized anxiety in teenagers.
Neurofeedback therapy for children with ADHD has been found to have minimal side effects, with most studies reporting no adverse effects. The treatment is generally well-tolerated, with children experiencing improvements in attention, impulse control, and hyperactivity. Some potential side effects that have been reported include mild headaches, fatigue, or dizziness, but these are typically temporary and resolve quickly. Additionally, neurofeedback therapy is non-invasive and does not involve the use of medication, making it a safe and appealing option for parents seeking alternative treatments for their children with ADHD. It is important for parents to consult with a qualified healthcare professional to determine if neurofeedback therapy is a suitable option for their child.