

Neurofeedback targets and addresses the symptoms of ADHD in adults by training the brain to regulate and optimize its own activity. Z-Score Neurofeedback By monitoring brainwave patterns, neurofeedback aims to modify specific frequencies associated with ADHD symptoms, such as impulsivity and inattention. Through operant conditioning, individuals learn to self-regulate their brainwave activity, leading to improved attention, impulse control, and executive function. This process helps adults with ADHD to retrain their brains and develop more efficient neural pathways, ultimately reducing the impact of their symptoms.
Neurofeedback for Anxiety Disorders (e.g., Social Anxiety, Generalized Anxiety)
The potential long-term benefits of neurofeedback therapy for adults with ADHD are promising. Research suggests that neurofeedback can lead to sustained improvements in attention, impulse control, and overall cognitive function. By targeting the underlying neural dysregulation associated with ADHD, neurofeedback has the potential to bring about lasting changes in brain function, providing individuals with enhanced self-regulation skills and improved daily functioning. These long-term benefits make neurofeedback a valuable option for adults seeking non-pharmacological interventions for ADHD.
Neurofeedback can be used as a standalone treatment for ADHD in adults, although it is often integrated with other therapies for comprehensive care. While neurofeedback has shown efficacy as a standalone intervention, combining it with other treatments, such as cognitive-behavioral therapy or lifestyle modifications, can enhance its overall effectiveness. Biofeedback Therapy This multidisciplinary approach addresses the diverse needs of adults with ADHD, offering a more holistic and personalized treatment plan.
Specific brainwave patterns that neurofeedback aims to modify in adults with ADHD include increased beta activity and enhanced theta/beta ratio. By increasing beta activity, individuals may experience improved focus and attention, while optimizing the theta/beta ratio can lead to reduced impulsivity and hyperactivity. Mindfulness These modifications in brainwave patterns can have a direct impact on ADHD symptoms, helping adults to achieve greater cognitive control and emotional regulation.
The typical duration and frequency of neurofeedback sessions for adults with ADHD can vary depending on individual needs and treatment plans. Generally, sessions may last 30-60 minutes and occur 1-3 times per week. Results from neurofeedback therapy can be expected within several weeks to months, with some individuals noticing improvements in attention and self-regulation early in the treatment process. Consistency and adherence to the recommended session schedule are crucial for maximizing the benefits of neurofeedback.
Skin Temperature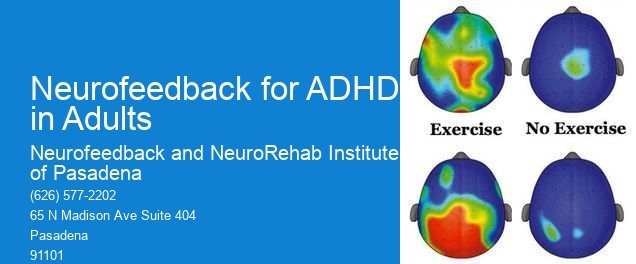
Potential side effects associated with neurofeedback therapy for adults with ADHD are minimal. Breath Control Some individuals may experience mild fatigue or temporary changes in mood following sessions, but these effects are typically short-lived. It's important for individuals considering neurofeedback to consult with a qualified provider to ensure that they are suitable candidates for this treatment. Contraindications may include certain neurological conditions or severe cognitive impairments, which should be carefully assessed before initiating neurofeedback therapy.
When comparing neurofeedback to traditional medication-based treatments for ADHD in adults, research suggests that both approaches can be effective, but they target different aspects of the condition. Neurofeedback offers a non-invasive, non-pharmacological alternative that focuses on directly training the brain to self-regulate, while medications primarily address neurotransmitter imbalances. While medication may provide more immediate symptom relief, neurofeedback has the potential for longer-lasting benefits and can be particularly beneficial for individuals seeking non-pharmacological options or those who experience side effects from medication. Ultimately, the choice between neurofeedback and medication should be based on individual preferences, treatment goals, and the guidance of healthcare professionals.
Research on the efficacy of neurofeedback for phobias has shown that there may be age-related differences in its effectiveness. Studies have indicated that younger individuals may respond more readily to neurofeedback interventions due to their greater neuroplasticity and ability to adapt to new learning experiences. Conversely, older individuals may require more sessions or a different approach to achieve similar results. Factors such as cognitive flexibility, attentional control, and emotional regulation may also play a role in determining the effectiveness of neurofeedback for phobias across different age groups. Further investigation into these age-related differences could provide valuable insights for optimizing neurofeedback protocols for individuals of all ages.
Neurofeedback strategies for improving learning disabilities often involve targeted protocols designed to enhance cognitive functions such as attention, memory, and executive functioning. These protocols may include sensorimotor rhythm (SMR) training, which aims to improve focus and attention, as well as beta and theta training to address issues related to impulsivity and distractibility. Additionally, protocols targeting specific brain regions associated with language processing, such as the left temporal lobe, may be utilized to address reading and language-based learning disabilities. By utilizing quantitative electroencephalography (qEEG) to identify individualized neurofeedback targets, practitioners can tailor interventions to address the specific neurophysiological underpinnings of each person's learning challenges. This personalized approach allows for the optimization of neurofeedback training to address the unique cognitive and neural dynamics associated with learning disabilities.
Neurofeedback therapy for depression may have contraindications and limitations that should be considered. Individuals with a history of epilepsy or seizure disorders may not be suitable candidates for neurofeedback due to the potential risk of triggering seizures. Additionally, those with certain neurological conditions or brain injuries may not benefit from or may even be at risk for adverse effects from neurofeedback therapy. It is important for healthcare providers to conduct a thorough assessment of each individual's medical history and current condition to determine the appropriateness of neurofeedback for treating depression. Furthermore, the effectiveness of neurofeedback therapy for depression may vary depending on the severity and underlying causes of the individual's depressive symptoms, and it may not be a suitable standalone treatment for all cases of depression. Therefore, a comprehensive treatment plan that may include other therapeutic modalities should be considered for optimal outcomes.
Neurofeedback, also known as EEG biofeedback, has shown promise in aiding stroke recovery and rehabilitation by targeting the brain's neuroplasticity and promoting functional reorganization. By utilizing real-time monitoring of brainwave activity, neurofeedback can help individuals with stroke-related impairments to enhance their cognitive and motor functions. This non-invasive technique involves providing feedback to the brain in the form of visual or auditory cues, which can help in improving attention, memory, and motor control. Through repeated sessions, neurofeedback can potentially facilitate the restoration of neural pathways and improve overall brain function, contributing to the recovery and rehabilitation process following a stroke.
Neurofeedback therapy is employed in children with Tourette's syndrome to help regulate and improve their brain function, reducing the frequency and severity of tics and other symptoms associated with the condition. By utilizing specialized equipment to monitor and provide real-time feedback on brainwave activity, neurofeedback therapy aims to train the brain to self-regulate and function more efficiently. This non-invasive approach focuses on enhancing neuroplasticity, promoting self-regulation, and optimizing neural connectivity. Through repetitive sessions, children with Tourette's syndrome can learn to modulate their brain activity, leading to improved symptom management and overall well-being. This personalized and targeted intervention can complement traditional treatments, offering a holistic approach to addressing the unique needs of children with Tourette's syndrome.
Neurofeedback has shown promise in providing relief from chronic migraine pain by utilizing biofeedback techniques to train individuals to regulate their brainwave patterns. By targeting specific neural pathways associated with pain perception and modulation, neurofeedback aims to modulate cortical excitability, enhance self-regulation, and promote neuroplasticity. This non-invasive approach involves real-time monitoring of brain activity and providing feedback to help individuals learn to self-regulate their brain function, potentially reducing the frequency and intensity of migraine attacks. Additionally, neurofeedback may also address comorbid conditions such as anxiety and stress, which are often associated with chronic migraine, offering a comprehensive approach to managing migraine symptoms. While further research is needed to fully establish its efficacy, neurofeedback presents a promising avenue for individuals seeking alternative or complementary treatments for chronic migraine pain.
Neurofeedback, a form of biofeedback that uses real-time monitoring of brain activity to teach self-regulation, has shown promise as an adjunctive treatment for managing symptoms of bipolar disorder. While it can be a valuable component of a comprehensive treatment plan, current evidence does not support its use as a sole intervention for managing bipolar disorder symptoms. However, neurofeedback may help individuals with bipolar disorder improve self-awareness, emotional regulation, and cognitive function, potentially complementing other therapeutic approaches such as medication, psychotherapy, and lifestyle modifications. Further research is needed to fully understand the potential benefits of neurofeedback in the management of bipolar disorder.