

Neurofeedback therapy targets the underlying neurological factors contributing to eating disorders by utilizing real-time monitoring of brainwave activity to train individuals to regulate their brain function. This form of therapy focuses on enhancing self-regulation and improving brain connectivity, which can help address the dysregulation in brain areas associated with eating disorders. By providing feedback to the individual about their brainwave patterns, neurofeedback aims to promote healthier neurological functioning, potentially reducing the symptoms and behaviors associated with eating disorders.
BiofeedbackNeurofeedback can be used as a standalone treatment for eating disorders, but it is often integrated with other therapies for a comprehensive approach. While neurofeedback may directly target the neurological aspects of eating disorders, combining it with other treatments such as cognitive-behavioral therapy, nutritional counseling, and support groups can address the multifaceted nature of eating disorders more effectively. This integrated approach can provide a more holistic treatment plan that addresses both the neurological and psychological aspects of the disorder.
The potential benefits of using neurofeedback as part of a comprehensive treatment plan for eating disorders include promoting self-regulation, reducing anxiety and depression symptoms, improving impulse control, and enhancing emotional regulation. By targeting the neurological underpinnings of eating disorders, neurofeedback may help individuals develop healthier coping mechanisms and reduce maladaptive behaviors related to disordered eating. Signal Processing Additionally, it may contribute to overall improvements in mental well-being and quality of life.
Neurofeedback has shown promise in addressing various types of eating disorders, including anorexia nervosa, bulimia nervosa, and binge-eating disorder. Research suggests that neurofeedback may be particularly effective in addressing the underlying neurological dysregulation associated with these disorders, potentially leading to improvements in symptoms such as obsessive thoughts about food, body image disturbances, and impulse control issues. EEG However, the effectiveness of neurofeedback may vary for each individual, and personalized treatment plans are essential.
In addition to targeting the neurological aspects of eating disorders, neurofeedback therapy also addresses the emotional and psychological components of these conditions. By promoting self-regulation and improving brain connectivity, neurofeedback may help individuals better manage emotional distress, reduce anxiety and depression symptoms, and enhance overall emotional resilience. This holistic approach aims to address the complex interplay between neurological, emotional, and psychological factors contributing to eating disorders.
EEG Biofeedback Software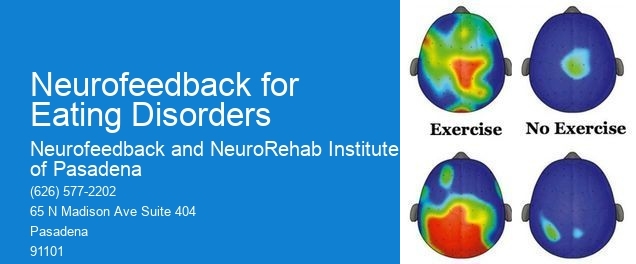
The typical duration and frequency of neurofeedback sessions for individuals with eating disorders can vary depending on the severity of the condition and individual response to treatment. Generally, neurofeedback sessions may range from 30 to 60 minutes and occur one to three times per week. The duration of treatment may span several months, with periodic assessments to monitor progress and adjust the treatment plan as needed. Personalized treatment plans are crucial to ensure the best outcomes for individuals with eating disorders.
When used under the guidance of qualified professionals, neurofeedback is considered safe for individuals with eating disorders. However, there are potential risks and contraindications to consider, such as the possibility of experiencing temporary discomfort or fatigue during or after sessions. Beta Waves Additionally, individuals with certain neurological conditions or those taking specific medications may not be suitable candidates for neurofeedback. It is essential for healthcare providers to conduct thorough assessments and consider individual circumstances before recommending neurofeedback as a treatment for eating disorders.

Yes, there are neurofeedback programs specifically designed to address the symptoms of Tourette's syndrome. These programs utilize neurofeedback techniques to target the specific neural pathways and brain activity associated with Tourette's syndrome, aiming to improve symptom management and overall quality of life for individuals with the condition. Neurofeedback protocols for Tourette's syndrome may focus on enhancing self-regulation of motor and vocal tics, reducing impulsivity, and promoting relaxation and emotional regulation. These programs often involve personalized treatment plans tailored to the individual's unique symptoms and needs, and may incorporate techniques such as electroencephalography (EEG) to monitor and train brainwave patterns. Additionally, neurofeedback for Tourette's syndrome may integrate cognitive-behavioral strategies to address associated challenges, such as attention deficits or anxiety. Overall, these specialized neurofeedback programs offer a targeted and holistic approach to supporting individuals with Tourette's syndrome in managing their symptoms and improving their daily functioning.
The typical duration of neurofeedback treatment for panic disorder can vary depending on the individual's response to the therapy, the severity of the symptoms, and the specific protocol used by the healthcare provider. Generally, neurofeedback treatment for panic disorder may involve regular sessions over a period of several months, with some individuals experiencing benefits after as few as 20 sessions, while others may require more extensive treatment. The frequency of sessions and the overall duration of treatment are often tailored to the unique needs and progress of each patient, with healthcare providers monitoring and adjusting the treatment plan as necessary to optimize outcomes. It's important for individuals considering neurofeedback for panic disorder to consult with a qualified healthcare professional to receive personalized guidance on the expected duration and potential benefits of this therapy.
Yes, there are specific neurofeedback protocols that can be tailored to address different eating disorders. For example, for anorexia nervosa, protocols may focus on increasing alpha and theta brainwave activity to promote relaxation and reduce anxiety, as well as enhancing executive function and emotional regulation. For bulimia nervosa, protocols may target reducing impulsivity and enhancing self-control, as well as addressing any underlying anxiety or depression. For binge eating disorder, protocols may aim to improve impulse control and reduce cravings, as well as addressing emotional dysregulation and stress management. These protocols can be customized based on the individual's specific symptoms and needs, and may involve a combination of neurofeedback training, cognitive-behavioral techniques, and mindfulness practices to address the complex nature of eating disorders.
The implementation of neurofeedback in pediatric epilepsy management may encounter several potential challenges. Firstly, the need for specialized training and expertise in neurofeedback techniques among healthcare professionals could pose a barrier to widespread adoption. Additionally, ensuring the safety and efficacy of neurofeedback interventions in pediatric patients with epilepsy requires rigorous monitoring and assessment protocols. Furthermore, the availability of resources and infrastructure for delivering neurofeedback therapy, such as access to advanced neuroimaging technology and specialized equipment, may present logistical challenges. Moreover, addressing the individual variability in treatment response and tailoring neurofeedback protocols to the specific needs of pediatric epilepsy patients necessitates a personalized and adaptive approach. Lastly, navigating regulatory and ethical considerations, as well as integrating neurofeedback into existing clinical practices, requires careful coordination and collaboration among multidisciplinary healthcare teams.
Neurofeedback treatment for adult ADHD carries potential risks, including the possibility of experiencing side effects such as headaches, fatigue, or dizziness. Additionally, there is a risk of not achieving the desired therapeutic outcomes, leading to frustration and disappointment. In some cases, individuals may also experience temporary worsening of symptoms before improvement is observed. It is important for individuals considering neurofeedback treatment to be aware of these potential risks and to discuss them with a qualified healthcare professional to make an informed decision about their treatment options.
Neurofeedback protocols used in substance use disorder treatment often include alpha-theta training, SMR (sensorimotor rhythm) training, and beta training. These protocols aim to address specific neurophysiological dysregulations associated with substance use disorder, such as impulsivity, emotional dysregulation, and executive function deficits. Alpha-theta training targets the enhancement of relaxation and emotional processing, while SMR training focuses on improving attention, impulse control, and emotional stability. Beta training aims to enhance cognitive function and reduce anxiety. Additionally, protocols may incorporate coherence training to improve communication between brain regions and promote overall brain function. These neurofeedback protocols are tailored to address the individual's specific neurobiological challenges and support their recovery from substance use disorder.