Neurofeedback therapy targets chronic pain management by training the brain to regulate its own activity, leading to reduced pain perception and improved pain tolerance. By using real-time monitoring of brainwave activity, neurofeedback helps individuals learn to self-regulate their brain function, which can lead to decreased pain intensity and improved overall well-being. This therapy specifically targets the brain's ability to modulate pain signals and can be a valuable tool in the comprehensive management of chronic pain.
Neurofeedback aims to address specific brainwave patterns such as increased theta and alpha activity, as well as decreased beta activity, in chronic pain patients. Training Protocols These patterns are often associated with heightened pain perception and reduced pain tolerance. By training individuals to modify these brainwave patterns through neurofeedback, the therapy seeks to normalize brain activity and reduce the experience of chronic pain.
Neurofeedback can be used as a standalone treatment for chronic pain, but it is often more effective when used in conjunction with other therapies such as physical therapy, medication management, and cognitive-behavioral therapy. When integrated into a comprehensive treatment plan, neurofeedback can enhance the overall effectiveness of chronic pain management and provide long-lasting benefits.
GSR
While neurofeedback therapy has shown promise in addressing various types of chronic pain conditions, it has demonstrated particularly promising results in conditions such as fibromyalgia, migraines, and neuropathic pain. Baseline These conditions often involve complex pain processing mechanisms, and neurofeedback can help individuals modulate their brain activity to better manage these types of chronic pain.
The potential long-term effects of neurofeedback therapy on chronic pain management include sustained reductions in pain intensity, improved pain coping mechanisms, and enhanced overall quality of life. Sensors By training the brain to self-regulate and modulate pain signals, individuals may experience lasting improvements in their chronic pain symptoms even after completing a course of neurofeedback therapy.
Neurofeedback therapy addresses the psychological aspects of chronic pain, such as anxiety and depression, by promoting relaxation, stress reduction, and emotional regulation. EMG By targeting specific brainwave patterns associated with these psychological states, neurofeedback can help individuals achieve a greater sense of calm and emotional well-being, which can in turn positively impact their experience of chronic pain.
There are specific protocols and guidelines for incorporating neurofeedback into a comprehensive chronic pain management plan. These may include initial assessments to identify individualized treatment targets, regular monitoring of progress through quantitative EEG analysis, and the integration of neurofeedback sessions with other therapeutic interventions. By following established protocols, healthcare providers can ensure that neurofeedback is effectively integrated into a holistic approach to chronic pain management.

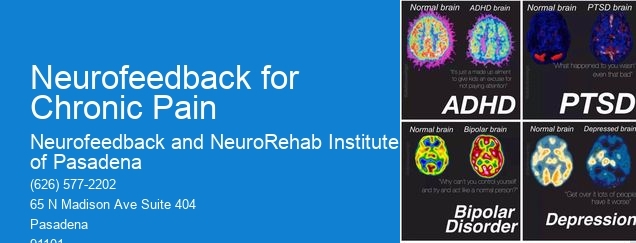
Neurofeedback therapy can be beneficial for individuals with bipolar disorder by helping to regulate and stabilize their brain activity. By using specialized equipment to monitor and provide feedback on brainwave patterns, neurofeedback therapy aims to train the brain to self-regulate and improve mood stability. This form of therapy can target specific brain regions associated with emotional regulation, attention, and impulse control, which are often affected in individuals with bipolar disorder. Through repeated sessions, individuals may experience improvements in mood swings, anxiety, and overall emotional well-being. Additionally, neurofeedback therapy may also enhance cognitive function and reduce the frequency and severity of manic and depressive episodes, providing a holistic approach to managing bipolar disorder symptoms.
Yes, there are neurofeedback programs specifically designed to help manage bipolar disorder. These programs utilize neurofeedback techniques, also known as EEG biofeedback, to train individuals to regulate their brain activity and improve mood stability. Neurofeedback for bipolar disorder typically focuses on enhancing self-regulation and reducing symptoms such as mood swings, impulsivity, and emotional dysregulation. These programs often incorporate personalized protocols tailored to the individual's specific brainwave patterns and symptoms, aiming to promote greater emotional balance and cognitive functioning. Additionally, neurofeedback for bipolar disorder may involve monitoring and training specific brain regions associated with mood regulation, such as the prefrontal cortex and limbic system. Overall, these specialized neurofeedback programs offer a promising approach to complement traditional treatments for bipolar disorder and may contribute to improved symptom management and overall well-being.
Neurofeedback has shown promise in addressing substance abuse and addiction by targeting the underlying neurological imbalances associated with these conditions. Research suggests that neurofeedback can help regulate brain activity, improve impulse control, and reduce cravings, thereby supporting individuals in their recovery journey. By utilizing advanced brainwave monitoring and feedback techniques, neurofeedback aims to enhance self-regulation and promote healthier patterns of brain function, potentially mitigating the risk of relapse. This non-invasive, personalized approach may complement traditional addiction treatment modalities, offering a holistic and neurologically tailored intervention for individuals seeking to overcome substance use disorders.
When considering the use of neurofeedback for postpartum depression, it is important to take into account the individual's specific symptoms, neurophysiological profile, and overall mental health history. Factors such as the severity of the depression, any co-occurring anxiety or mood disorders, and the presence of any underlying medical conditions should be carefully assessed. Additionally, the potential benefits and risks of neurofeedback as a treatment modality, including its effectiveness in regulating brain activity, should be thoroughly evaluated. It is also crucial to consider the expertise and qualifications of the healthcare professionals administering the neurofeedback, as well as the availability of appropriate resources and support for the individual undergoing treatment. Overall, a comprehensive and personalized approach that takes into consideration the unique needs and circumstances of the individual is essential when using neurofeedback for postpartum depression.
Neurofeedback, also known as EEG biofeedback, plays a significant role in managing ADHD symptoms in children and adolescents. This non-invasive treatment method involves training individuals to regulate their brainwave patterns, targeting specific areas associated with attention, impulse control, and executive function. By providing real-time feedback on brain activity, neurofeedback helps individuals learn to self-regulate and improve cognitive functioning. Research has shown that neurofeedback can lead to reductions in ADHD symptoms, such as hyperactivity, impulsivity, and inattention, and can also enhance academic performance and social behavior. It offers a promising alternative or complementary approach to traditional ADHD treatments, promoting long-term improvements in neurocognitive functioning and overall well-being.
Neurofeedback therapy has shown promise in benefiting individuals with borderline personality disorder (BPD) across various age groups. Research suggests that neurofeedback, a form of biofeedback that targets brain activity, may help regulate emotional dysregulation, impulsivity, and cognitive functioning in individuals with BPD. Studies have indicated that neurofeedback training can lead to improvements in emotional stability, self-regulation, and overall quality of life for both adolescents and adults with BPD. Furthermore, neurofeedback interventions have demonstrated efficacy in addressing specific symptoms such as mood instability, interpersonal difficulties, and identity disturbance, offering potential benefits for individuals of different age ranges within the BPD population. Overall, the evidence suggests that neurofeedback therapy holds promise as a complementary approach for addressing the multifaceted challenges associated with BPD across diverse age groups.