

Neurofeedback therapy targets the neurological mechanisms involved in migraines by focusing on regulating brainwave activity. Specifically, it aims to modify the abnormal patterns of brainwave activity associated with migraines, such as increased theta and decreased alpha and beta waves. By using real-time monitoring of brainwave activity, neurofeedback helps individuals learn to self-regulate their brainwave patterns, leading to improved neurological function and reduced migraine frequency and severity.
The specific brainwave patterns that neurofeedback aims to modify in order to reduce migraine frequency and severity include increasing the amplitude of alpha and beta waves while decreasing the amplitude of theta waves. Alpha waves are associated with relaxation and calmness, while beta waves are linked to focused attention and cognitive processing. QEEG (Quantitative EEG) By training individuals to increase these beneficial brainwave patterns and decrease the abnormal theta wave activity, neurofeedback aims to create a more balanced and stable neurological state, which can help reduce the occurrence and intensity of migraines.
Neurofeedback can be used as a standalone treatment for migraines, although it is often integrated with other therapies for comprehensive management. While some individuals may experience significant relief from migraines through neurofeedback alone, others may benefit from a combination of neurofeedback with lifestyle modifications, medication, or other complementary treatments. The decision to use neurofeedback as a standalone or adjunctive therapy is typically based on the individual's unique needs and the severity of their migraines.
Specific protocols and techniques used in neurofeedback therapy are tailored to address the unique neurological aspects of migraines. This may involve targeting specific brain regions or networks that are implicated in migraine pathophysiology, such as the prefrontal cortex, insula, or default mode network. Additionally, personalized neurofeedback protocols are designed based on each individual's brainwave patterns and symptom presentation, ensuring a targeted and individualized approach to migraine management.
Neurofeedback TrainingScientific evidence supports the effectiveness of neurofeedback in managing migraines, with several studies and clinical trials demonstrating its benefits. Research has shown that neurofeedback can lead to significant reductions in migraine frequency, intensity, and duration, as well as improvements in overall quality of life for migraine sufferers. These findings contribute to the growing recognition of neurofeedback as a valuable non-pharmacological intervention for migraine management.
Thresholds
The timeline for noticeable improvements in migraine symptoms with neurofeedback therapy can vary among individuals. Some may experience relief within a few weeks of starting neurofeedback sessions, while others may require several months to achieve significant and lasting improvements. The results of neurofeedback therapy for migraines are often reported as long-lasting, with many individuals experiencing sustained benefits even after completing their neurofeedback training.
Stress ReductionPractitioners providing neurofeedback therapy for migraines should have specific qualifications and certifications to ensure their expertise in this specialized area. Look for practitioners who are licensed healthcare professionals, such as psychologists, neurotherapists, or neurofeedback specialists, with additional training and certification in neurofeedback for migraine management. Temperature Biofeedback Patients seeking a qualified provider should also consider the practitioner's experience, expertise, and track record in treating migraines with neurofeedback.
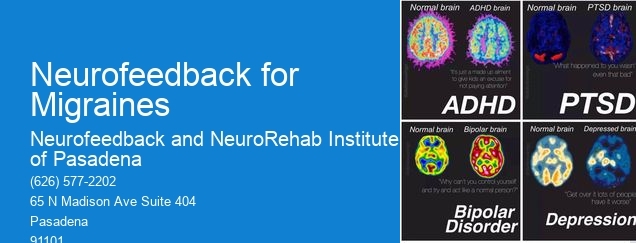
Neurofeedback therapy has shown promising results in reducing symptoms of social anxiety in teenagers. By utilizing advanced neuroimaging techniques, neurofeedback therapy targets specific brain regions associated with anxiety, such as the amygdala and prefrontal cortex, to regulate emotional responses and cognitive processes. This personalized approach allows adolescents to learn self-regulation techniques, enhancing their ability to manage social anxiety symptoms. Furthermore, neurofeedback therapy incorporates biofeedback mechanisms, enabling individuals to gain awareness and control over physiological responses, contributing to a holistic reduction in social anxiety symptoms. Research indicates that neurofeedback therapy can lead to long-term improvements in social anxiety symptoms, offering teenagers a valuable tool for managing and overcoming their challenges in social situations.
Yes, neurofeedback can be utilized as an adjunct therapy for trauma-related disorders. Neurofeedback, also known as EEG biofeedback, is a non-invasive technique that aims to regulate brain activity by providing real-time feedback on brainwave patterns. Research has shown that neurofeedback can help individuals with trauma-related disorders by targeting specific brain regions associated with emotional regulation, arousal, and stress response. By training the brain to self-regulate and modulate its activity, neurofeedback can potentially reduce symptoms such as anxiety, hypervigilance, and emotional dysregulation commonly seen in trauma-related disorders. Additionally, neurofeedback can complement traditional therapies by addressing underlying neurobiological dysregulation, offering a holistic approach to treatment. Its potential as an adjunct therapy for trauma-related disorders is supported by a growing body of evidence and clinical applications.
Neurofeedback techniques for treatment-resistant depression in adults encompass a range of approaches, including electroencephalography (EEG) biofeedback, real-time functional magnetic resonance imaging (rtfMRI) neurofeedback, and quantitative electroencephalography (qEEG) training. These techniques aim to modulate brain activity and promote self-regulation of neural function by providing real-time feedback on brainwave patterns. Neurofeedback protocols may target specific brain regions or networks implicated in depression, such as the prefrontal cortex, anterior cingulate cortex, or default mode network. Additionally, personalized neurofeedback training may involve enhancing alpha and theta brainwave activity, promoting connectivity within neural circuits, and fostering emotional regulation and resilience. Integrating neurofeedback with traditional treatments, such as medication and psychotherapy, can offer a comprehensive approach to addressing treatment-resistant depression in adults.
Neurofeedback, also known as EEG biofeedback, has shown promise in assisting individuals with managing complex trauma-related disorders. By utilizing real-time monitoring of brainwave activity, neurofeedback aims to help regulate and optimize brain function, potentially addressing symptoms such as anxiety, depression, and PTSD. This non-invasive technique involves providing feedback to the individual about their brainwave patterns, allowing them to learn self-regulation and potentially alleviate symptoms associated with trauma-related disorders. Research suggests that neurofeedback may help modulate the dysregulated neural networks often observed in individuals with complex trauma, offering a potential avenue for addressing the underlying neurobiological mechanisms contributing to these conditions. While further studies are needed to fully elucidate its efficacy, neurofeedback presents a promising adjunctive approach in the comprehensive management of complex trauma-related disorders.
Neurofeedback has shown promise in addressing complex trauma disorders with comorbid conditions by targeting specific neural pathways associated with trauma responses, such as hyperarousal, dissociation, and emotional dysregulation. By utilizing real-time monitoring of brain activity and providing feedback to the individual, neurofeedback can help regulate the autonomic nervous system, enhance emotional regulation, and improve cognitive functioning. Additionally, neurofeedback can address comorbid conditions such as anxiety, depression, and attention-deficit/hyperactivity disorder by promoting neuroplasticity and optimizing brain functioning. This approach offers a personalized and non-invasive intervention that complements traditional therapeutic modalities, providing a holistic approach to addressing complex trauma disorders and their associated comorbidities.