Neurofeedback targets Parkinson's disease symptoms by aiming to regulate and optimize brainwave activity, particularly in the areas of the brain associated with motor control and movement. By using real-time monitoring of brainwave patterns, neurofeedback can help individuals with Parkinson's disease learn to self-regulate their brain activity, potentially leading to improvements in motor function and symptom management.
The most common neurofeedback techniques used for managing Parkinson's disease symptoms include sensorimotor rhythm (SMR) training, beta training, and alpha-theta training. SMR training focuses on enhancing the brainwave frequencies associated with motor control, while beta training aims to regulate the beta brainwave activity related to movement and coordination. Alpha-theta training targets the alpha and theta brainwave frequencies to promote relaxation and reduce stress, which can indirectly impact motor function in individuals with Parkinson's disease.
Heart Rate Variability BiofeedbackNeurofeedback has shown promise in improving motor function in individuals with Parkinson's disease. By training the brain to regulate specific brainwave patterns associated with motor control, neurofeedback may help enhance coordination, reduce tremors, and improve overall movement abilities. However, individual responses to neurofeedback may vary, and the extent of improvement can differ from person to person.
Feedback Display
Specific brainwave patterns targeted by neurofeedback to alleviate Parkinson's disease symptoms include the regulation of beta and SMR frequencies. By optimizing these brainwave patterns, neurofeedback aims to enhance motor control, reduce tremors, and improve overall movement abilities in individuals with Parkinson's disease.
The timeline for seeing improvements in Parkinson's disease symptoms with neurofeedback therapy can vary depending on individual factors such as the severity of symptoms, the frequency of neurofeedback sessions, and the individual's responsiveness to the treatment. Some individuals may experience noticeable improvements within a few weeks of starting neurofeedback therapy, while others may require several months to achieve significant benefits.
Alpha Waves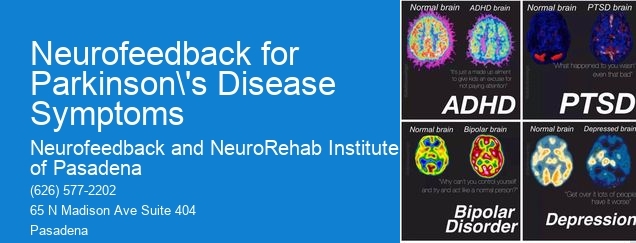
When used under the guidance of trained professionals, neurofeedback for Parkinson's disease symptoms is generally considered safe and well-tolerated. Biofeedback Research However, as with any therapeutic intervention, there may be potential side effects or risks, such as temporary fatigue, mild headaches, or temporary changes in mood. It's essential for individuals considering neurofeedback for Parkinson's disease to consult with qualified healthcare providers to discuss potential risks and benefits.
Current research evidence supporting the effectiveness of neurofeedback for managing Parkinson's disease symptoms is promising but still evolving. Several studies have demonstrated positive outcomes in terms of motor function, quality of life, and symptom management in individuals with Parkinson's disease. Peak Performance However, more extensive clinical trials and long-term studies are needed to further establish the efficacy of neurofeedback as a complementary approach for managing Parkinson's disease symptoms.

Neurofeedback therapy has shown promise in addressing tinnitus-related distress by targeting the underlying neural mechanisms associated with the condition. By utilizing real-time monitoring of brainwave activity and providing feedback to the individual, neurofeedback aims to modulate neural networks and improve self-regulation of auditory processing. This approach may help reduce the perception of tinnitus, alleviate associated anxiety and stress, and enhance overall quality of life for individuals experiencing tinnitus-related distress. Additionally, neurofeedback therapy may involve techniques such as alpha-theta training, coherence training, and sensorimotor rhythm training, which are tailored to address specific aspects of tinnitus-related distress. Overall, neurofeedback therapy offers a non-invasive and potentially effective intervention for managing the impact of tinnitus on psychological well-being.
Neurofeedback has garnered attention as a potential treatment for panic disorder, with emerging evidence suggesting its efficacy. Studies have shown that neurofeedback, a form of biofeedback that aims to regulate brain activity, can help individuals with panic disorder gain better control over their physiological responses to stress and anxiety. By targeting specific brainwave patterns associated with panic symptoms, neurofeedback may help individuals learn to self-regulate their emotional and physiological responses, leading to a reduction in panic attacks and overall symptom severity. Furthermore, neurofeedback has been found to have a positive impact on related factors such as anxiety, stress, and overall quality of life. While more research is needed to fully establish its effectiveness, the preliminary findings support the potential of neurofeedback as a valuable adjunctive treatment for panic disorder.
Neurofeedback approaches for addressing treatment-resistant depression may include techniques such as electroencephalography (EEG) biofeedback, neurostimulation, and real-time functional magnetic resonance imaging (rtfMRI) neurofeedback. These approaches aim to modulate brain activity and regulate neural networks associated with mood regulation, emotional processing, and cognitive function. Additionally, protocols involving alpha-theta training, sensorimotor rhythm (SMR) training, and low-frequency repetitive transcranial magnetic stimulation (rTMS) may be utilized to target specific brain regions and neural oscillations implicated in depression. Furthermore, personalized neurofeedback protocols tailored to individual neurophysiological patterns and symptom profiles may be employed to enhance treatment efficacy and address the unique neurobiological underpinnings of treatment-resistant depression.
Neurofeedback for postpartum depression during breastfeeding presents unique challenges due to the need to consider the impact of the treatment on both the mother and the infant. The practitioner must carefully monitor the effects of neurofeedback on the mother's mental health while ensuring that it does not interfere with breastfeeding or affect the infant's well-being. Factors such as hormone levels, sleep patterns, and stress management become crucial in tailoring the neurofeedback protocol to address the specific needs of the postpartum mother. Additionally, the practitioner may need to collaborate with lactation consultants and mental health professionals to provide comprehensive support for the mother's overall well-being. It is essential to approach neurofeedback for postpartum depression during breastfeeding with a holistic understanding of the interconnectedness of the mother-infant dyad and the specific challenges it presents.
Yes, there are specialized neurofeedback protocols designed specifically for Parkinson's disease patients. These protocols often focus on targeting the specific neural pathways and brain regions affected by Parkinson's disease, such as the basal ganglia and motor cortex. Neurofeedback training for Parkinson's disease may involve protocols that aim to improve motor function, reduce tremors, enhance cognitive function, and address non-motor symptoms such as depression and anxiety. These protocols may utilize techniques such as sensorimotor rhythm (SMR) training, beta training, and coherence training to address the unique neurological challenges presented by Parkinson's disease. Additionally, personalized neurofeedback protocols may be tailored to the individual needs and symptoms of each Parkinson's disease patient, taking into account factors such as disease progression, medication effects, and comorbidities.