

Neurofeedback therapy targets the symptoms of bipolar disorder by aiming to regulate the brainwave patterns associated with the condition. Galvanic Skin Response Biofeedback By using real-time monitoring of brain activity, neurofeedback helps individuals with bipolar disorder learn to self-regulate their brain function, potentially reducing symptoms such as mood swings, impulsivity, and emotional dysregulation. This therapy focuses on enhancing self-awareness and self-regulation, which can be particularly beneficial for individuals with bipolar disorder.
The potential benefits of using neurofeedback as a complementary treatment for bipolar disorder are numerous. Neurofeedback may help individuals with bipolar disorder gain better control over their emotional and cognitive processes, leading to improved mood stability and reduced severity of mood episodes. Additionally, it can potentially enhance the effectiveness of other treatments, such as medication and psychotherapy, by addressing underlying brainwave dysregulation.
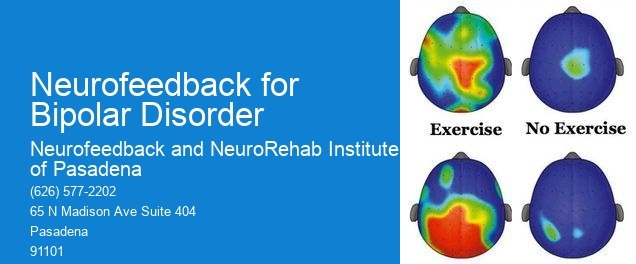
Neurofeedback aims to regulate specific brainwave patterns, such as alpha, beta, theta, and delta waves, in individuals with bipolar disorder. Respiration Rate By targeting these patterns, neurofeedback seeks to promote greater balance and stability in brain function, which may contribute to improved emotional regulation and overall well-being for individuals with bipolar disorder.
In contrast to traditional medication-based treatments for bipolar disorder, neurofeedback offers a non-invasive and drug-free approach. While medication primarily focuses on managing symptoms through chemical intervention, neurofeedback aims to address the underlying brainwave dysregulation that contributes to bipolar disorder symptoms. Skin Conductance This approach may be particularly appealing to individuals who prefer non-pharmacological treatments or who experience side effects from medication.
Research evidence supports the effectiveness of neurofeedback in managing bipolar disorder symptoms. Studies have shown that neurofeedback can lead to improvements in mood stability, reduced severity of mood episodes, and enhanced emotional regulation in individuals with bipolar disorder. While more research is needed, the existing evidence suggests that neurofeedback may be a valuable addition to the treatment options for bipolar disorder.

Potential risks or side effects associated with neurofeedback therapy for individuals with bipolar disorder are generally minimal. Some individuals may experience temporary fatigue or mild discomfort during or after neurofeedback sessions, but these effects are typically short-lived. It's important for individuals considering neurofeedback to consult with a qualified healthcare professional to discuss any potential concerns and determine if neurofeedback is a suitable treatment option for them.
Feedback DisplayThe process of neurofeedback therapy for bipolar disorder typically begins with an initial assessment to evaluate the individual's symptoms, brainwave patterns, and overall suitability for neurofeedback. Following the assessment, individuals undergo a series of neurofeedback sessions, during which they receive real-time feedback on their brainwave activity and learn to self-regulate their brain function. Neuroplasticity Ongoing sessions are tailored to the individual's progress and may involve adjustments based on their response to the therapy. Throughout the process, individuals work closely with trained professionals to optimize the benefits of neurofeedback for managing their bipolar disorder symptoms.
Neurofeedback therapy has emerged as a promising alternative for managing adult ADHD, offering a non-invasive approach that targets the brain's neural activity. By utilizing real-time monitoring of brainwave patterns, neurofeedback aims to train individuals to regulate their brain function, potentially reducing symptoms associated with ADHD. This therapy involves the use of specialized equipment to provide feedback on brainwave activity, allowing individuals to learn self-regulation techniques. Research suggests that neurofeedback may help improve attention, impulse control, and executive function in adults with ADHD. While it may not entirely replace medication for some individuals, neurofeedback therapy can be a valuable adjunct or alternative treatment option, particularly for those seeking non-pharmacological interventions. It is important for individuals considering neurofeedback to consult with qualified healthcare professionals to determine its suitability and potential benefits in their specific case.
Neurofeedback has shown promise in providing pain relief for individuals with chronic pain conditions. By utilizing electroencephalography (EEG) to measure brainwave activity, neurofeedback aims to train the brain to regulate its responses to pain stimuli. This process involves providing real-time feedback to the individual, allowing them to learn how to modulate their brainwave patterns and potentially reduce their perception of pain. Studies have indicated that neurofeedback may help individuals with chronic pain conditions, such as fibromyalgia, neuropathic pain, and migraines, by promoting neuroplasticity and altering pain processing pathways. While further research is needed to fully understand its efficacy, neurofeedback presents a promising avenue for managing chronic pain and improving overall quality of life for those affected.
Neurofeedback strategies for treating different types of phobias vary based on the specific nature of the phobia. For instance, in the case of specific phobias such as arachnophobia or acrophobia, neurofeedback may focus on desensitization techniques to reduce the exaggerated fear response associated with the specific trigger. On the other hand, for social phobias or agoraphobia, neurofeedback may target regulating the brain's response to anxiety and stress, promoting relaxation and reducing the hyperarousal associated with these phobias. Additionally, for complex phobias, such as those related to trauma or PTSD, neurofeedback may involve addressing underlying emotional dysregulation and reactivity patterns. Overall, the neurofeedback approach is tailored to address the unique neural and emotional processes underlying each type of phobia, aiming to promote adaptive brain functioning and reduce the impact of the phobia on the individual's daily life.
Neurofeedback, also known as EEG biofeedback, has shown promising results in the treatment of generalized anxiety disorder (GAD). Research studies have indicated that neurofeedback can be effective in reducing anxiety symptoms by training individuals to regulate their brainwave patterns. While success rates can vary depending on individual factors such as severity of symptoms, commitment to treatment, and the specific neurofeedback protocol used, many studies have reported significant improvements in anxiety levels following neurofeedback therapy. Additionally, neurofeedback has been found to have lasting effects, with some individuals experiencing continued reduction in anxiety symptoms even after the completion of treatment. It is important to note that neurofeedback is often used as part of a comprehensive treatment plan for GAD, and its effectiveness may be enhanced when combined with other therapeutic interventions such as cognitive-behavioral therapy or medication.
Neurofeedback techniques for addressing Parkinson's disease tremors may involve protocols that focus on enhancing motor control, reducing muscle rigidity, and improving overall brain function. Specific neurofeedback protocols may target the sensorimotor cortex, basal ganglia, and supplementary motor area to modulate neural activity related to tremors. Additionally, neurofeedback training may aim to optimize beta and gamma oscillations, enhance coherence between brain regions, and promote neuroplasticity to mitigate tremor symptoms. By utilizing real-time monitoring of brainwave activity and providing feedback to the individual, neurofeedback can help retrain neural pathways and improve motor function in individuals with Parkinson's disease. Furthermore, personalized neurofeedback protocols may incorporate techniques such as coherence training, SMR (sensorimotor rhythm) enhancement, and alpha-theta training to address tremors and associated symptoms.
Neurofeedback is a non-invasive therapeutic approach that targets specific symptoms of panic disorder by training the brain to regulate its activity. By utilizing electroencephalography (EEG) to monitor brainwave patterns, neurofeedback helps individuals with panic disorder to recognize and self-regulate their physiological responses to stress and anxiety. This process involves providing real-time feedback to the individual, allowing them to learn how to modulate their brainwave activity and reduce symptoms such as hyperventilation, palpitations, and feelings of impending doom. Through repeated sessions, neurofeedback aims to retrain the brain to achieve a more balanced and resilient state, ultimately reducing the frequency and intensity of panic attacks. Additionally, neurofeedback can address comorbid symptoms such as insomnia, muscle tension, and cognitive distortions, offering a comprehensive approach to managing panic disorder.
Neurofeedback protocols for social anxiety in teenagers may differ from those for adults due to the unique developmental and cognitive factors at play. When designing protocols for teenagers, practitioners may consider incorporating age-appropriate feedback mechanisms and targeting specific neural networks associated with adolescent social cognition and emotional regulation. Additionally, the protocols may emphasize building skills for managing peer interactions and navigating social challenges commonly faced during adolescence. In contrast, protocols for adults may focus on addressing long-standing patterns of social anxiety and may involve targeting different neural pathways and cognitive processes. Tailoring neurofeedback protocols to the specific developmental stage and cognitive needs of the individual can optimize the effectiveness of the intervention for social anxiety in both teenagers and adults.